Frontal Lobe Dementia Gambling
What is frontal lobe dementia?
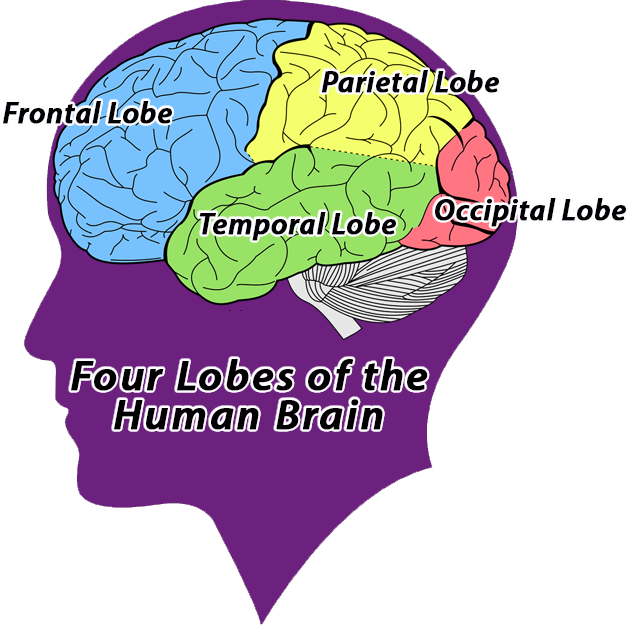
The frontal lobes of the brain are located as the name suggests at the front of the brain. Loosely speaking, it contains what we call the higher functions of the brain. These are the areas of the brain responsible for emotions, understanding, speech; some types of movement, planning and judgement in other words the things which make you a person, and personality. Like all dementias the people who develop symptoms face a slow loss of self and those who care for them, losing the person they care for by slow degrees.
- A study by Suwa Tokyo University of Science showed that elderly who gamble demonstrated a small increase in activity in the brain’s frontal and parietal lobes and displayed better recognition. More and more Japanese elders are gambling playing games like baccarat, mahjong, pachinko, and slot machines.
- About 10 – 15% of dementia cases are thought to be frontal lobe dementia, the disease affecting 1 in 5000 of the population. However in those under 65 it is believed to be 20 – 50% of cases. Onset of frontal lobe dementia is normally identified when the patient is between 45 and 65 years of age, although it has been seen in people aged 20.
Frontal lobe dementia is also known as frontotemporal dementia (FTD), or frontotemporal degeneration, it is an overarching term for several categories of a loss of brain function. The changes to the brain are caused by an abnormal build-up of tau proteins, which stop the brain cells from functioning properly, so they die. In frontal lobe dementia parts of the frontal and temporal lobes of the brain are damaged. It was previously known as ‘Pick’s disease’ after the doctor Arnold Pick who identified and first documented the symptoms in a patient over a hundred years’ ago in 1892.
Frontal Lobe Dementia Gambling Disorder
Unlike the most widely diagnosed form of dementia, Alzheimer’s disease, frontal lobe dementia occurs at a much younger age and is partly genetic. That means while there is no certainty that if you have had a close blood relative with FLD you will get it too, your chances of developing it are much higher than for other members of the population.
There are several genes that appear to link with frontal lobe dementia, which ties in with a family history of the disease being the only known risk factor. Approximately 15% of people diagnosed have a family member with the disease. However there is no single cause for the disease.
There are three predominant forms of frontal lobe dementia:
Frontotemporal dementia is an umbrella term for a group of uncommon brain disorders that primarily affect the frontal and temporal lobes of the brain. These areas of the brain are generally associated with personality, behavior and language. In frontotemporal dementia, portions of these lobes shrink (atrophy). Frontotemporal dementia is sometimes called frontal lobe dementia. It used to be known as Pick’s disease, after Arnold Pick the physician who discovered it. What are the symptoms of frontotemporal.
- Behavioural variant frontotemporal dementia, affecting approximately two thirds of people with the disease. Besides changes in behaviour, people with this form will find it difficult to control, plan or organise their actions.
- Progressive non-fluent aphasia, where the areas controlling speech in the temporal lobe are damaged. People will find it difficult to speak and eventually become mute.
- Semantic dementia, where the areas of the temporal lobe responsible for the understanding of language and knowledge are damaged. People will have problems with thinking and language.
In approximately 20% of cases, there is frontotemporal dementia also associated with motor neurone disease (MND), where in addition the nerve cells that control voluntary movement in the body are destroyed, resulting in people with the disease gradually losing the ability to move. Professor Steven Hawking is perhaps the most well-known personality to have developed a form of MND.
Signs and symptoms?
As with other forms of dementia, frontal lobe dementia is progressive, increasingly affecting behaviour and emotion, language, and ability to think or problem solve. People with the disease may have problems with speaking or understanding speech. Depending upon which parts of the frontal lobe are damaged first they may become very enthusiastic or display apathy. When the centres responsible for control of decision making are affected first they may also display inappropriate behaviour. There are other causes of these changes which are not FTL dementia related, but these are usually a result of injury or trauma which have affected the same part of the brain, the most well-known case being Phineas Gage a railway engineer who suffered left frontal lobe damage as a result of being impaled on a spike following an explosion.
NHS Choices lists the following signs for frontotemporal dementia:
- inappropriate behaviour in public
- impulsivity
- loss of inhibitions
- overeating, a change in food preferences (such as suddenly liking sweet foods), poor table manners
- neglect of personal hygiene
- repetitive or obsessional behaviours, such as humming, hand-rubbing and foot-tapping, or complex routines such as walking exactly the same route repetitively
- seeming more selfish
- inability to empathise with others, seeming cold and uncaring
- irritability
- being tactless or rude
- being less or more outgoing than in the past
- being lethargic, lacking enthusiasm
- depression
Whilst the tau protein build-up and damage seen at post mortem, a magnetic resonance imaging scan (MRI) will show the shrinkage in the lobes to assist diagnosis. Diagnosis is normally made after a series of physical and mental assessments, and diagnostic tests to rule out other causes.
Life expectancy and Treatment
About 10 – 15% of dementia cases are thought to be frontal lobe dementia, the disease affecting 1 in 5000 of the population. However in those under 65 it is believed to be 20 – 50% of cases. Onset of frontal lobe dementia is normally identified when the patient is between 45 and 65 years of age, although it has been seen in people aged 20 to 30 years of age. Only 10% of cases are identified in those 70 years and over.
The disease takes from three to ten years to progress, although there are instances of much shorter or longer times. The average life expectancy of a person diagnosed with frontal lobe dementia is eight years. Approximately 50% of deaths are as a result of pneumonia, following complications associated with inability of the person to move or care for themselves.
As with other forms of dementia there is no current cure for the disease, but there are a range of treatments that can help to manage and deal with the symptoms, and to help people to regain some of their lost functions.
These include drugs such as SSRI antidepressants to help control the symptoms like obsession, over-eating and depression. Antipsychotics may be given to address challenging and inappropriate behaviours. Psychological treatments such as cognitive stimulation and behavioural therapy can help maintain memory function address anxiety. Rehabilitative practices such as, occupational therapy, physiotherapy and speech therapy can help the brain to learn new ways to do things.
Frontal Lobe Dementia Gambling Disorders
At the time of writing, the best hope for a cure or enhanced length of life, lies with stem cell research but this is still at an early stage and a long way from clinical trials.
People with the disease will need a range of services as it progresses and a multi-disciplinary care plan needs to be established soon after diagnosis and revised as the person experiences more symptoms.
The distinction between the various forms of the disease becomes less obvious as the disease progresses. For example all people with the disease will lose some or all of their speech. In the latter stages the symptoms are very similar to those of Alzheimer’s disease and the person will need full time care.
References:

(Source: http://www.nhs.uk/Conditions/frontotemporal-dementia/Pages/Symptoms.aspx)
What is frontotemporal dementia?
Frontotemporal dementia (FTD), a common cause of dementia, is a group of disorders that occur when nerve cells in the frontal and temporal lobes of the brain are lost. This causes the lobes to shrink. FTD can affect behavior, personality, language, and movement.
These disorders are among the most common dementias that strike at younger ages. Symptoms typically start between the ages of 40 and 65, but FTD can strike young adults and those who are older. FTD affects men and women equally.
The most common types of FTD are:
- Frontal variant. This form of FTD affects behavior and personality.
- Primary progressive aphasia. Aphasia means difficulty communicating. This form has two subtypes:
- Progressive nonfluent aphasia, which affects the ability to speak.
- Semantic dementia, which affects the ability to use and understand language.
A less common form of FTD affects movement, causing symptoms similar to Parkinson disease or amyotrophic lateral sclerosis (Lou Gehrig’s disease).
What causes frontotemporal dementia?
The cause of FTD is unknown. Researchers have linked certain subtypes of FTD to mutations on several genes. Some people with FTD have tiny structures, called Pick bodies, in their brain cells. Pick bodies contain an abnormal amount or type of protein.
What are the risks for frontotemporal dementia?
A family history of FTD is the only known risk for these diseases. Although experts believe that some cases of FTD are inherited, most people with FTD have no family history of it or other types of dementia.
What are the symptoms of frontotemporal dementia?
Symptoms of FTD start gradually and progress steadily, and in some cases, rapidly. They vary from person to person, depending on the areas of the brain involved. These are common symptoms:
- Behavior and/or dramatic personality changes, such as swearing, stealing, increased interest in sex, or a deterioration in personal hygiene habits
- Socially inappropriate, impulsive, or repetitive behaviors
- Impaired judgment
- Apathy
- Lack of empathy
- Decreased self awareness
- Loss of interest in normal daily activities
- Emotional withdrawal from others
- Loss of energy and motivation
- Inability to use or understand language; this may include difficulty naming objects, expressing words, or understanding the meanings of words
- Hesitation when speaking
- Less frequent speech
- Distractibility
- Trouble planning and organizing
- Frequent mood changes
- Agitation
- Increasing dependence
Some people have physical symptoms, such as tremors, muscle spasms or weakness, rigidity, poor coordination and/or balance, or difficulty swallowing. Psychiatric symptoms, such as hallucinations or delusions, also may occur, although these are not as common as behavioral and language changes.
How is frontotemporal dementia diagnosed?
Family members are often the first to notice subtle changes in behavior or language skills. It’s important to see a healthcare provider as early as possible to discuss:
- Symptoms, when they began, and how often they occur
- Medical history and previous medical problems
- Medical histories of family members
- Prescription medicines, over-the-counter medicines, and dietary supplements taken
No single test can diagnose FTD. Typically, healthcare providers will order routine blood tests and perform physical exams to rule out other conditions that cause similar symptoms. If they suspect dementia, they may:
- Evaluate neurological status health including reflexes, muscle strength, muscle tone, sense of touch and sight, coordination, and balance
- Assess neuropsychological status such as memory, problem-solving ability, attention span and counting skills, and language abilities
- Order magnetic resonance imaging (MRI) or computed tomography (CT) scans of the brain
How is frontotemporal dementia treated?
Currently, no treatments are available to cure or slow the progression of FTD, but healthcare providers may prescribe medicine to treat symptoms. Antidepressants may help treat anxiety and control obsessive-compulsive behaviors and other symptoms. Prescription sleeping aids can help ease insomnia and other sleep disturbances. Antipsychotic medicine may reduce irrational and compulsive behaviors.
Behavior modification may help control unacceptable or risky behaviors.
Speech and language pathologists and physical and occupational therapists can help adjustment to some of the changes caused by FTD.
What are the complications of frontotemporal dementia?
FTD is not life-threatening ─ people may live with it for years. But it can lead to an increased risk for other illnesses that can be more serious. Pneumonia is the most common cause of death, with FTD. People are also at increased risk for infections and fall-related injuries.
As FTD progressively worsens, people may engage in dangerous behaviors or be unable to care for themselves. They may need 24-hour nursing care or to stay in an assisted living facility or nursing home.
Living with frontotemporal dementia
Coping with FTD can be frightening, frustrating, and embarrassing for the patient and family members. Since some symptoms can’t be controlled, family members shouldn't take their loved one’s behaviors personally. Families need to maintain their own well-being, while ensuring that their loved one is treated with dignity and respect.
Caregivers should learn all they can about FTD and gather a team of experts to help the family meet the medical, financial, and emotional challenges they are facing.
It’s important to find a healthcare provider knowledgeable about FTD. Other healthcare specialists who may play a role on the team are home care nurses, neuropsychologists, genetic counselors, speech and language therapists, as well as physical and occupational therapists. Social workers can help the patient and caregivers find community resources, such as medical supplies and equipment, nursing care, support groups, respite care, and financial assistance.
Attorneys and financial advisors can help families prepare for the later stages of the disease.
Frontal Lobe Dementia Gambling Addiction
Advanced planning will help smooth future transitions for the patient and family members, and may allow all to participate in the decision-making process.
Little solid evidence exists that antioxidants and other supplements help those with FTD. You and your family members should talk with your healthcare provider about whether to try antioxidants and other supplements, such as coenzyme Q10, vitamin E, vitamin C, and B vitamins to support brain health.
When should I call my healthcare provider?
If you are diagnosed with FTD, you and your caregivers should talk with your healthcare providers about when to call them. Your healthcare provider will likely advise calling if your symptoms become worse, or if you have obvious or sudden changes in behavior, personality, or speech. This includes mood changes, such as increasing depression or feeling suicidal.
It can be very stressful for a caregiver to take care of a loved one with FTD. It's normal to have feelings of denial, anger, and irritability. Caregivers may also have anxiety, depression, exhaustion, and health problems of their own. Caregivers should contact their healthcare provider if they have any of these signs of stress.
Key points
- Frontotemporal dementia is a group of disorders characterized by the loss of nerve cells in the frontal and temporal lobes of the brain, which causes these lobes to shrink. The cause of FTD is unknown.
- Symptoms typically first occur between the ages of 40 and 65 and can include changes in personality and behavior, progressive loss of speech and language skills, and sometimes physical symptoms such as tremors or spasms.
- FTD tends to progress over time. Treatments can't cure the disease, but some medicines and other treatments, such as speech therapy can sometimes help with symptoms. If you have FTD, you may eventually need full-time nursing care, or to stay in an assisted living facility or nursing home.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.